The Long Term Plan for the NHS which was published today (7 Jan 2019) has been welcomed by health leaders in the North Cumbria Health and Care System.
The plan, which sets out a blueprint to make the NHS fit for the future, focuses on prevention, improving services for patients and the importance of integrating services to make them more effective and efficient.
More information can be found here www.england.nhs.uk/2019/01/long-term-plan/ and the full plan is available at www.longtermplan.nhs.uk/
Stephen Eames, the chief executive of North Cumbria University Hospitals NHS Trust (NCUH) and Cumbria partnership NHS Foundation Trust (CPFT) is also the leader of the North Cumbria Health and Care System. He said: “The long term plan gives a clear commitment to integrating health services so the patient is at the heart of our NHS. This is something we have been working towards for some time across north Cumbria and I am delighted that we are at the leading edge of our future NHS.”
North Cumbria Health and Care System was named as one of 14 exemplar areas in May 2018 when we were identified as a developing Integrated Care System. Every area across England will now be asked to work towards this model of integrating health services across primary care, the community and hospital services.
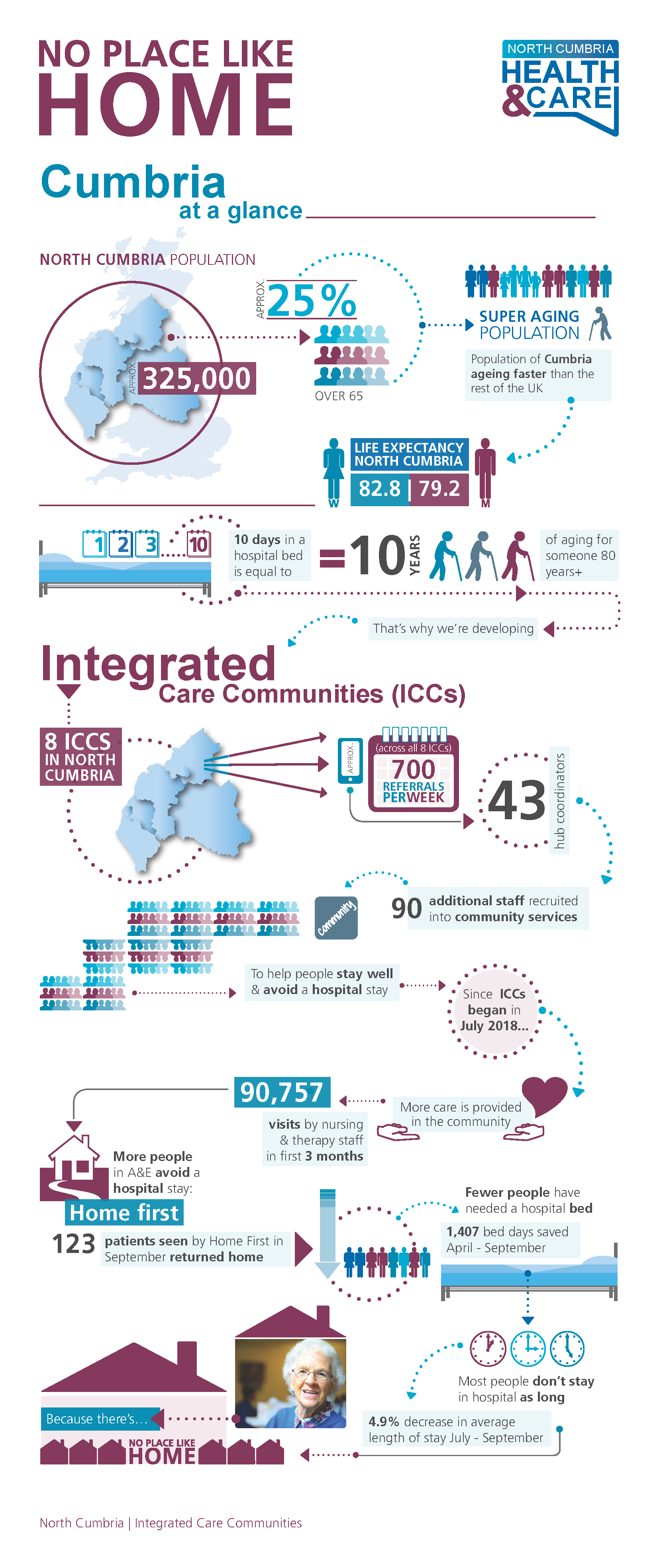
In north Cumbria we have developed 8 Integrated Care Communities (ICCs) where health and social care professionals, GPs, the third and voluntary sector and the community are increasingly working as one team to support the health and wellbeing of local people. This has included creating 90 new jobs and developing coordination hubs, rapid response service, frailty co-ordinators, and the lead practitioner of the day able to make clinical decisions on next steps in patient care without delay.
There is clear evidence that integration is having an impact already. We have probably seen the most progress in Alston where enhanced community services have been up and running for some time. They are now undertaking three times more visits in the community. This means more patients are avoiding hospital stays and receiving the appropriate care at home. Across north Cumbria, additional staff working in the community have enabled us to carry out over 90,000 visits since July 2018 which is helping people stay at home as set out in the case studies below.
Where people do come into hospital, we are often able to return them home more quickly, sometimes on the same day. Patients who are acutely unwell do need hospital care. When this happens we aim to get patients home as soon as it’s safe to do so as evidence shows that people often recover quicker at home.
Case Study 1
A man from Maryport spent a number of weeks at West Cumberland Hospital but was keen to go home. He was well enough to leave but still needed IV medication for a further 40 days. Thanks to the new day services at Maryport Hospital, he was able to return home and visit Maryport Hospital daily for the treatment – recovering in the comfort of his own home and saving the family a daily drive to Whitehaven
Case Study 2
The hub was contacted by a Palliative Care Social worker regarding someone on a hospital ward at the end of their life. The patient was deteriorating fast and had been clear their choice of place to die was home. The hub was able to liaise with the rapid response team who were able to identify the equipment and support needed to enable the patient to go home that day, the patient died the following day. Previously this may have taken several days to co-ordinate.
Access the NHS Elect toolkit by clicking this link: https://www.media.nhselect.nhs.uk/ldgwh/ldgwh.php